What’s a Rich Text element?
The rich text element allows you to create and format headings, paragraphs, blockquotes, images, and video all in one place instead of having to add and format them individually. Just double-click and easily create content.
Static and dynamic content editing
A rich text element can be used with static or dynamic content. For static content, just drop it into any page and begin editing. For dynamic content, add a rich text field to any collection and then connect a rich text element to that field in the settings panel. Voila!
How to customize formatting for each rich text
Headings, paragraphs, blockquotes, figures, images, and figure captions can all be styled after a class is added to the rich text element using the "When inside of" nested selector system.
- This is it.
Introduction
With expectations of an economic downturn on the horizon, many organisations are looking to do more with less. This is particularly true for large public organisations like the NHS. Whilst private businesses might experience reduced demand in an economic downturn, public healthcare bodies like the NHS are unlikely to face any drop in demand. In fact, with an ageing population, they will likely be expected to treat a growing number of patients every year. Any reduction in economic activity and related tax revenues will only tighten the budget available to take on that challenge.
Optimising Resource Allocation in the NHS
One way the NHS can do more with less is to allocate its existing resources optimally. In today’s blog, we will demonstrate how a Digital Twin of a hospital, built on the Silico business process simulation platform, can help organisations such as the NHS to do just that.
A Digital Twin of a hospital is a simulation model that forecasts how waiting lists, waiting times, required staff, financial resources and other KPIs of a hospital will develop over time, under different scenarios, and with different hospital policies and targets. This allows for senior decision-makers in hospitals and the NHS to test out decisions in a virtual environment before implementing them in the real world. They can make evidence-based decisions around things like the allocation of budgets (to hospitals and regions) and staff allocation within those hospitals so that specific targets, such as ED or surgery waiting times, are met as efficiently as possible. These simulations allow decision-makers to gain foresight of the real ramifications of a certain decision or combination of decisions, will likely be. This allows them to find the set of actions that will achieve the best possible outcomes for patients, given the ever-present constraints of budget and staff.
We’ve created a simplified Digital Twin of a hospital that can be used to allocate staff between a hospital’s Surgery and Emergency department. In this blog post, we’ll explore the value of these kinds of simulations and how they could and indeed have been used as decision-support tools for managers of hospitals and budget allocators within the NHS. In our next blog post, we will dive into building such a Digital Twin.
Using Silico to Optimise Resource Allocation in the NHS
So, let’s start with the dashboard of this “Hospital Twin” in Silico, seen below:
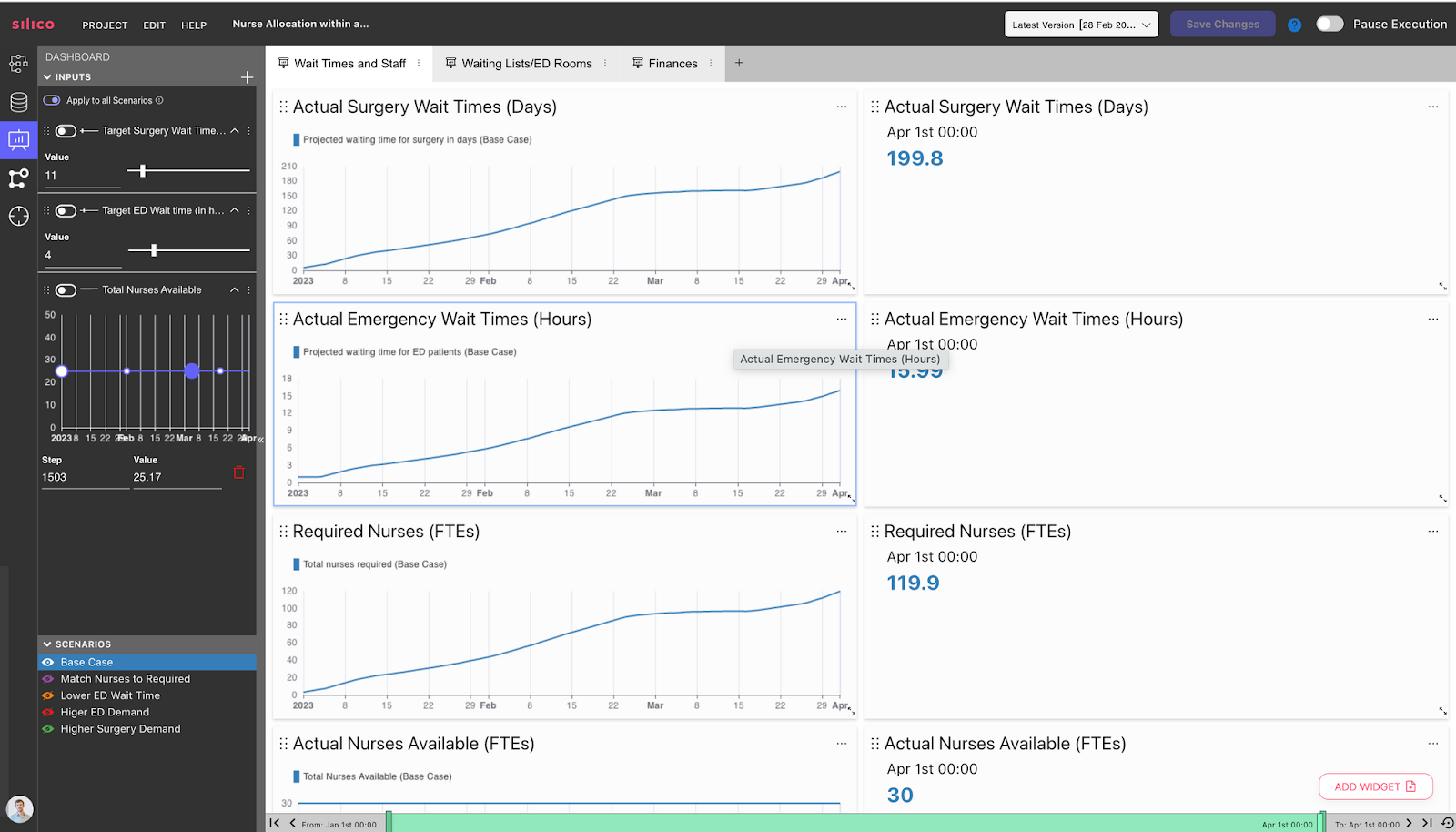
This dashboard has been designed for a decision-maker who is responsible for allocating nurses between a hospital’s Emergency department and Surgery departments daily. Decision-makers can alter the following inputs on the left, over which they have some control in real life:
- Target wait times for surgery, i.e. how long patients wait between being put on the surgery list and getting surgery.
- Target wait times for ED, i.e. how long patients wait between turning up at the ED and being treated/omitted.
- Total nurses available, controllable through hiring etc.
In the outputs section of the dashboard on the right, decision-makers see simulated, forward-looking results of essential KPIs of the hospital:
- Actual wait times for ED and surgery patients
- Required nurses to achieve target wait times
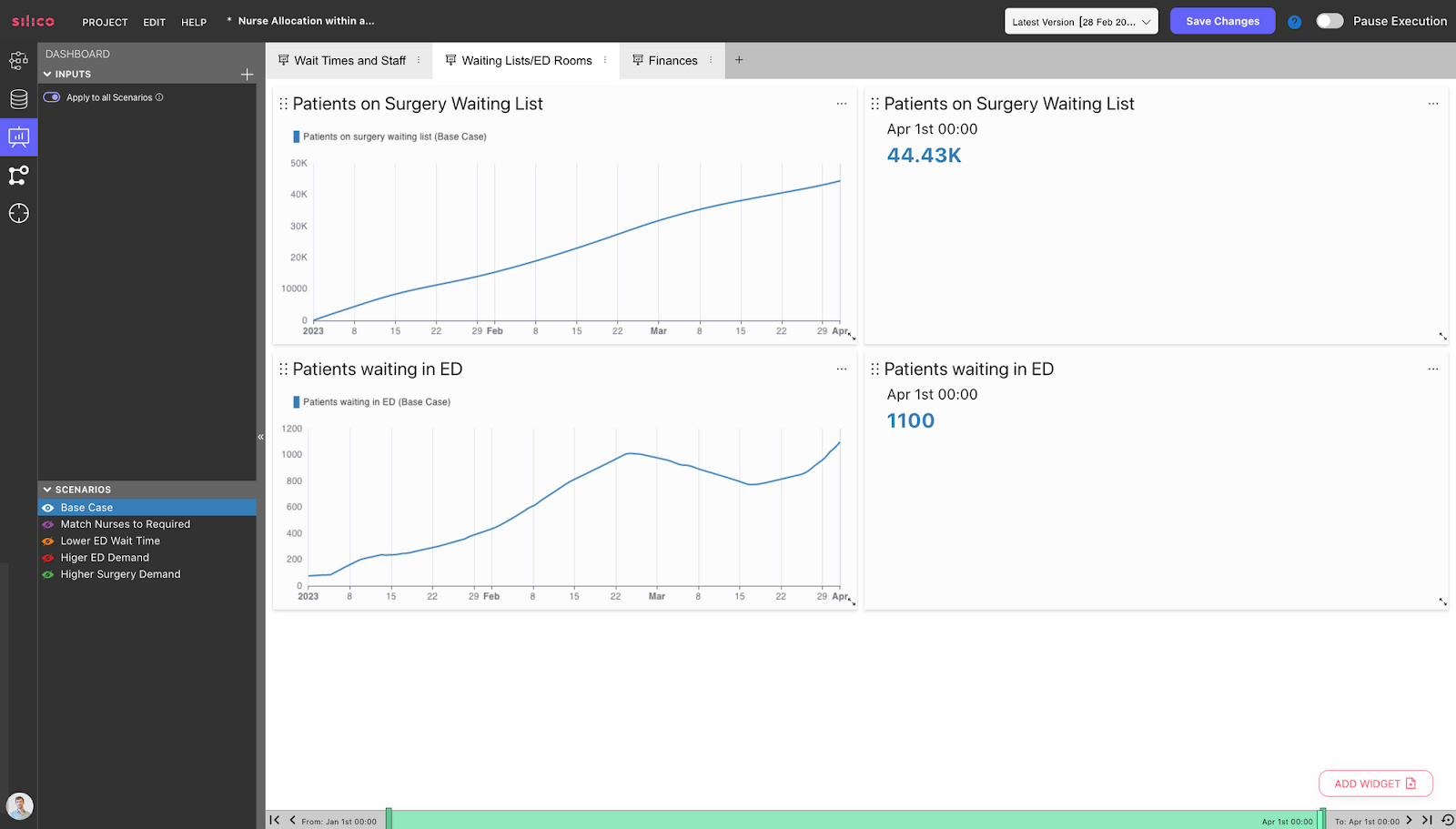
And on other dashboards, you can see:
- Surgery waiting lists
- Patients waiting in ED
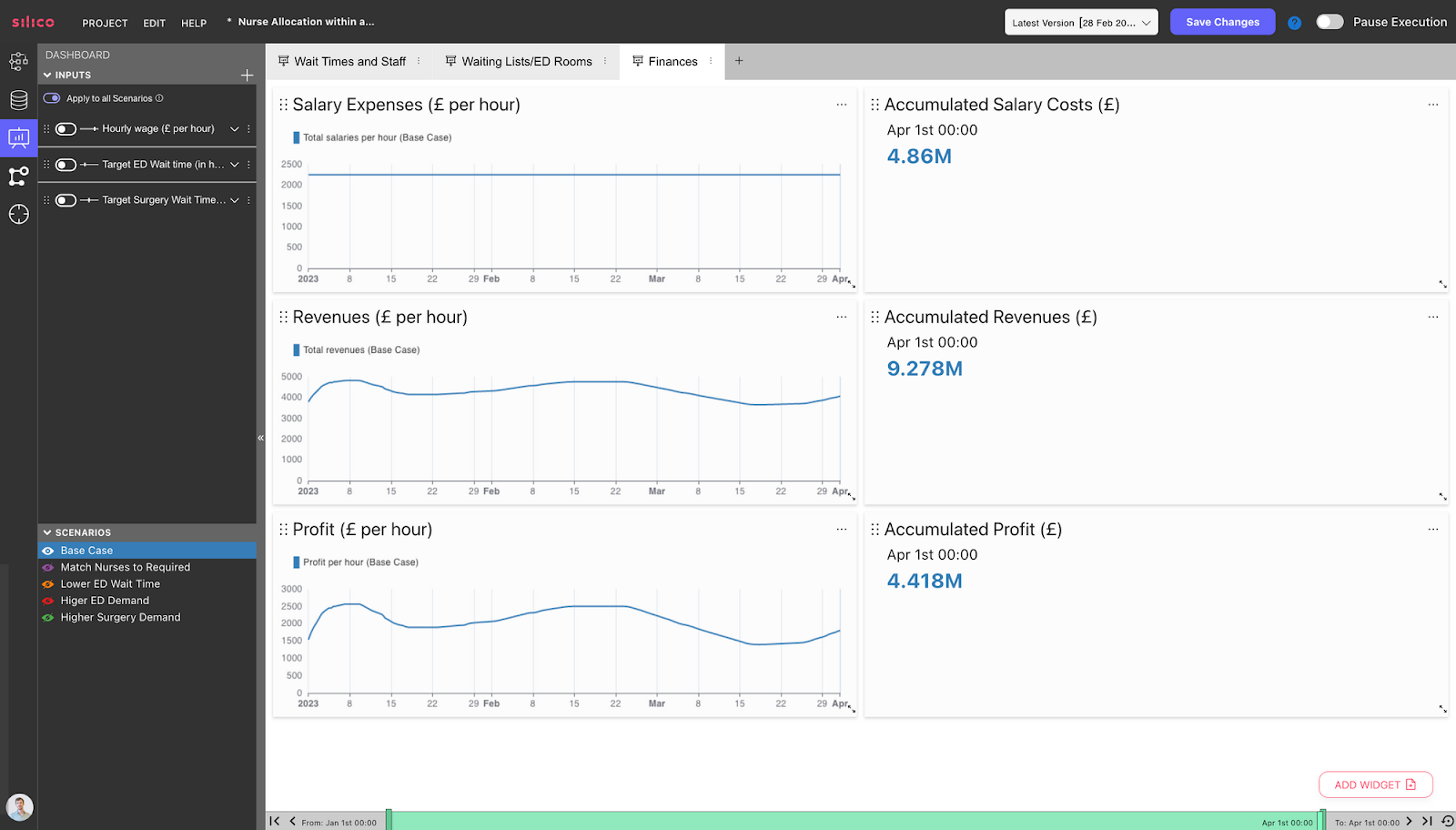
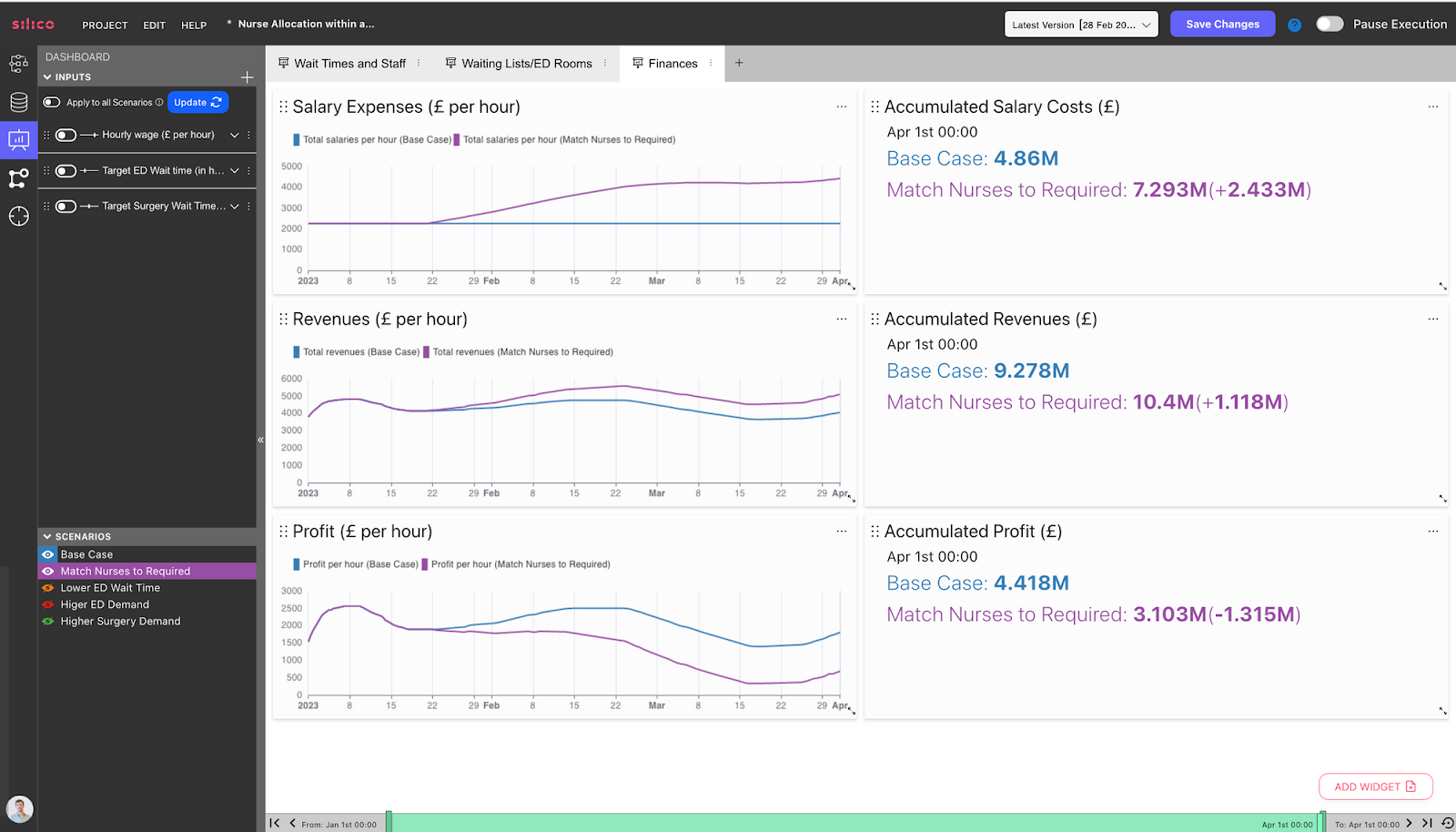
Hospital Digital Twins can easily connect to financial inputs for your hospital, such as staff pay per hour and revenue per patient treated. These inputs can be adjusted depending on the funding model of your hospital. We see a dashboard showing the revenues, expenses, and profits of the hospital:
By setting different input values, decision-makers can see how those decisions would impact the hospital’s KPIs. For example, let’s test out the decision to decrease the “Target ED waiting time” from 4 hours to 30 minutes, shown by the Orange Scenario below:
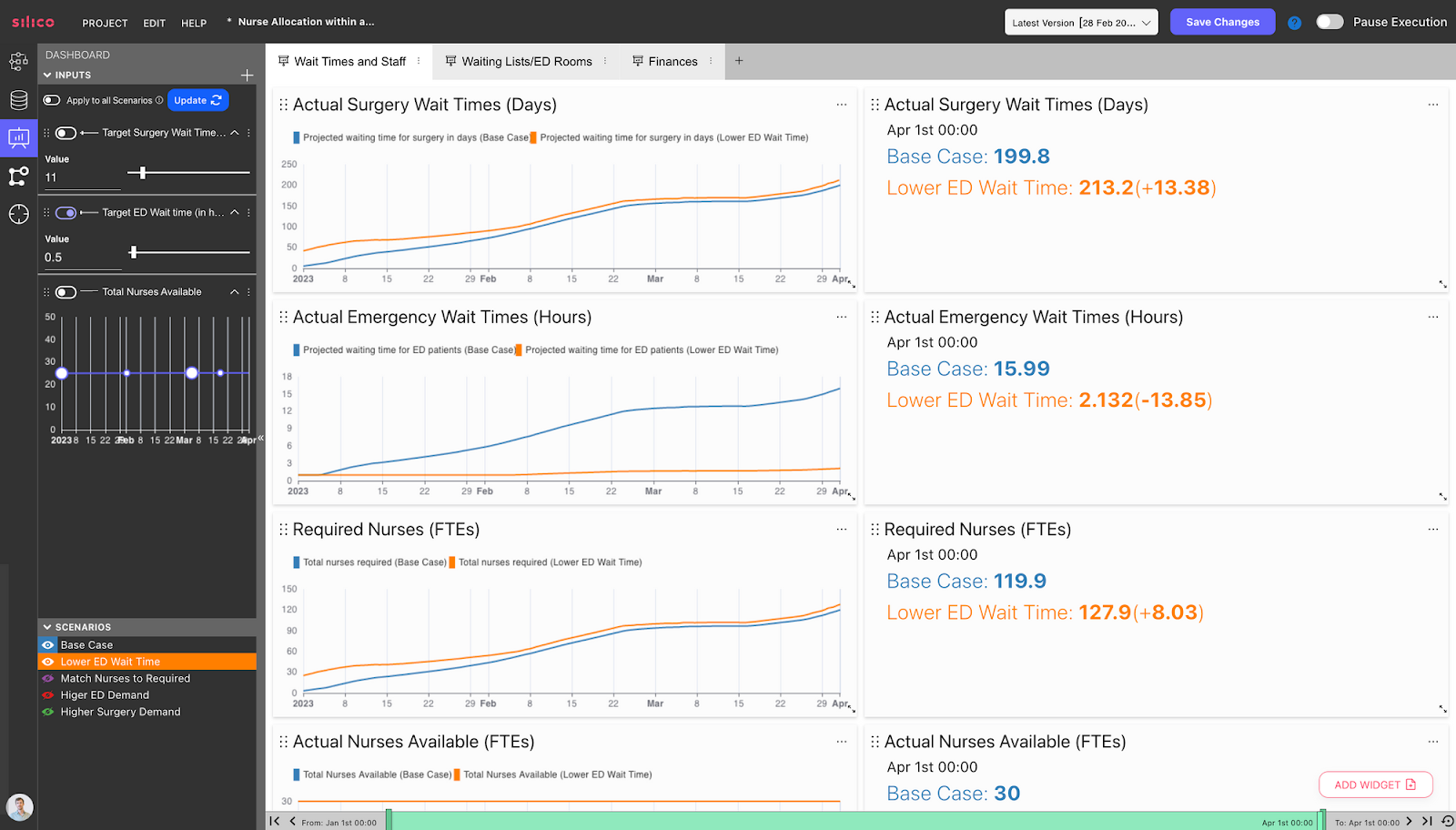
We can then see how this reduces ED waiting times and increases surgery wait times. This is because the underlying model reflects how nurses will be allocated to different departments based on these targets. For example, suppose the target times of the ED department are reduced without a proportional reduction in the target times for the surgery department. In that case, that change will increase performance in the ED department at the expense of the surgery department. Why? Because in this case, the corresponding increase in resources allocated to ED comes at the cost of resources allocated to surgery.
In addition, we have also seen that by the end of the simulation period, 8 nurses will be required to meet the target times, compared to the Base Case where ED target time was 4 hours instead of 30 minutes.
Let’s test another decision. Let’s say an NHS budget allocator wants to see what the cost would be to achieve the target times for ED and surgery of this hospital. To do this, we’ve created the purple Scenario in which the nurses will equal the nurses required to achieve target times.
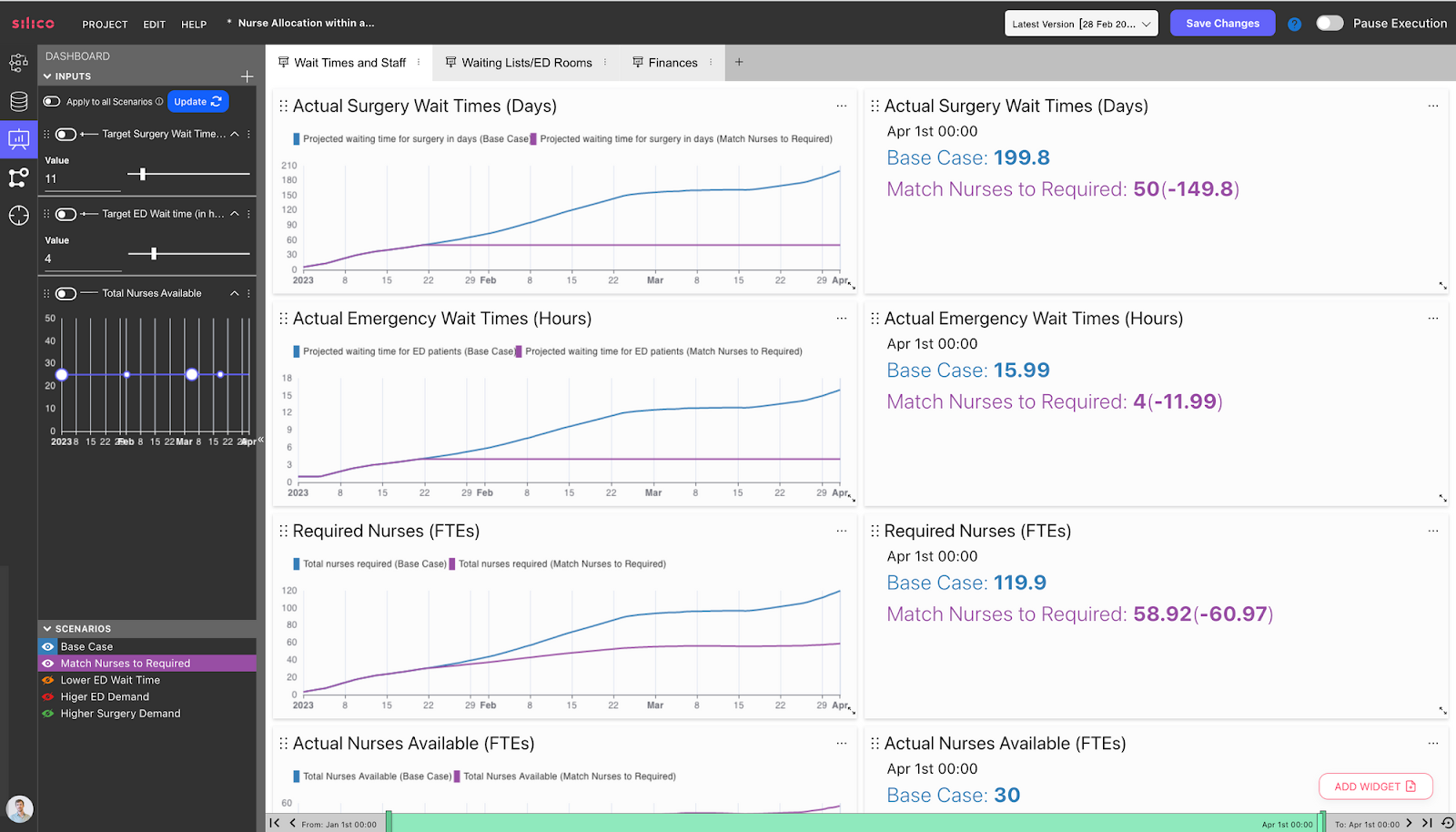
Note that in this Scenario, the required number of nurses at the end of the simulation period is lower than in the Base Case, where there were insufficient nurses available. This is because when insufficient nurses are available, the waiting lists and corresponding waiting times grow. This means that further nurses will be needed by the end of the simulation period if the hospital is to get back to a state where they can meet target wait times. This gives a clear understanding of the impacts of underinvesting today, allowing decision-makers to have a clear foresight of the long-term impacts of such decisions.
Below we can see the financial implications of the decision to match nurses to the required targets. Accumulated salary costs are £2.43 million pounds higher by the end of the simulation period. However, the hospital's profit is not as negatively affected thanks to an increase in revenues, due to more patients being treated, which counteracts the higher salary costs.
Of course, these models must be rigorously tested and validated before they can be used as robust decision-support tools. One of the most important tests compares the model’s simulations of the past with the actual historical data from that time period. For example, you could compare the model’s simulations of the number of patients on the surgery waiting list in May of 2022, with that actual data from that period. If there is a sufficiently close match between the two, then that gives greater confidence that the model’s future simulations will also give sound projections for the impact of certain decisions. Of course, no model can predict the future, but making the best projections possible is necessary to find the optimal decisions to manage the increasing complexity of healthcare in the UK and worldwide. Healthcare systems are highly complex, and simulation is necessary to understand that complexity and how decisions you implement will play out in the system.
Conclusion
To conclude, this blog has focused on the value that a Digital Twin of a Hospital can deliver. In essence, they help decision-makers make the most informed decisions possible on questions such as the right target times for each department, how many nurses to hire, and what the allocation of those nurses should be between departments. They can also use these simulations in negotiations of NHS budget allocation, to give a clear evidence basis for the required budget to achieve objectives.
In our next blog, we will describe the model that underlies the dashboard that was seen today, to explain how this value is delivered.

